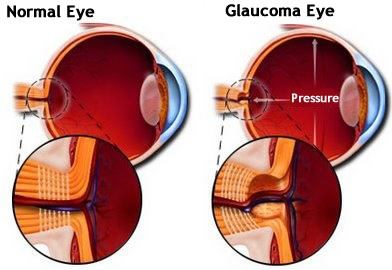
Intraocular pressure is the pressure mainly created by the continual renewal of fluids within the eyes. The intraocular pressure is increased in glaucoma. Eye pressure is mainly measured in millimeters of mercury (mm Hg). Normal eye pressure ranges from 10-21 mm Hg. Normal Intraocular pressure is an eye pressure of greater than 21 mm Hg. In acute angle-closure glaucoma, the intraocular pressure rises because the canal into which the fluid in the front part of the eyes normally drains is suddenly blocked. In chronic glaucoma, there is a gradual imbalance between the production and removal of the fluid in the back part of the eyes.
Eye Pressure Symptoms and Causes
Eye pressure causes are numerous. Factors that cause or are associated with Intraocular Pressure are virtually the same as the causes of glaucoma. These include:
Excessive Aqueous Production
The aqueous is the clear fluid that is produced in eyes by the ciliary body, a structure located behind the iris. Aqueous flows directly through the pupil and fills the anterior chamber of eyes, which is the space between the cornea and the iris.
The aqueous drains from the eyes through a structure called the trabecular meshwork, in the periphery of the anterior chamber, where iris and the cornea meet. If the ciliary body produces too much aqueous, the pressure in the eye increases, causing Intraocular Pressure.

Inadequate Aqueous Drainage
If the aqueous drains extremely slowly from the eyes, disrupting the normal balance of the production and drainage of eye’s clear fluid, this too will cause high eye pressure.
Certain medications can have the side effect of causing Intraocular Pressure in certain individuals. Steroid medicines utilized to treat asthma and other conditions have been shown to enhance the risk for Intraocular Pressure. Even steroid eye drops utilized after LASIK and other refractive surgery can cause high eye pressure in susceptible individuals.
Eye Trauma
An injury to the eyes can affect the balance of aqueous production and drainage from the eye, possibly leading to Intraocular Pressure. Many times this can occur months or years after the injury. During your routine eye exam, be sure to mention to your eye doctor if you have experienced any eye trauma in the past.
Several Other Eye Conditions
Intraocular Pressure has been associated with a number of other eye conditions, including pigment dispersion syndrome, pseudoexfoliation syndrome, and corneal arcus. If you have any of these conditions, the eye doctor may recommend that you have more frequent eye exams and eye pressure measurements.
Eye Pressure Symptoms
Most individuals with Intraocular Pressure do not experience any symptoms. For this reason, regular eye examination with an ophthalmologist is important to rule out any damage to the optic nerve from high pressure.

Eye Pressure Treatment
If your ophthalmologist prescribes medicines to aid in lowering the pressure inside the eyes, properly applying the medication and complying with the doctor’s instructions are very important. Not doing so could result in a further increase in intraocular pressure that can lead to permanent vision loss and optic nerve damage. Intraocular pressure treatment depends on your ophthalmologist. How the ophthalmologist chooses to treat you is highly individualized.
- Many ophthalmologists treat elevated intraocular pressure of higher than 21 mm Hg with topical medicines. Some do not medically treat unless there is an evidence of optic nerve damage. Most ophthalmologists treat if pressure is consistently higher than 28-30 mm Hg because of the high risk of optic nerve damage.

- If one is experiencing symptoms like blurred vision, halos or pain, or if one’s intraocular pressure has recently enhanced and then continues to increase on subsequent visits, the ophthalmologist will most likely commence medical treatment.
Intraocular pressure is evaluated periodically. One guideline to how often intraocular pressure is checked is given below.
- If one’s intraocular pressure is 28 mm Hg or higher, one is treated with medicines. After 1 month of taking the drug, one has a follow-up visit with the ophthalmologist to see if the medicines are lowering the pressure and there is no side effect. If the drug is working, then follow-up visits are scheduled every 4-5 months.
- If intraocular pressure is 26-27 mm Hg, the pressure is rechecked in 3-4 weeks after your initial visit. On the second visit, if the pressure is within 3 mm Hg of the reading at the initial visit, thereafter follow-up visits are scheduled every 4-5 months. If the pressure is lower on the second visit, then the length of time between follow-up visits is longer and is determined by the ophthalmologist.
- If your intraocular pressure is 22-25 mm Hg, the pressure is rechecked in 3-4 months. At the second visit, if the pressure is within 3 mm Hg of reading at the initial visit, then your next visit is in 8 months and includes visual field testing and an optic nerve examination. Testing is repeated at least yearly.
Laser and surgical therapy are not used to treat intraocular pressure because risks associated with these therapies are higher than the risk of developing glaucomatous damage from intraocular pressure.
